- Chronic Care
- Arthritis
Gout Treatment
Gout treatment available online today
In order to treat your gout, consult with one of our board-certified doctors online today to get a prescription to get rid of joint pain. Get a new prescription to treat gout or refill an existing prescription today.*
Book an appointmentEase pain, redness, and swelling
Manage gout symptoms conveniently
Quick and effective gout diagnosis
*Prescriptions are provided at the doctor's discretion. Learn more about our controlled substances policy and how to save up to 80% with our prescription discount card. PlushCare doctors cannot treat all cases of gout. Our primary care physicians can conduct an initial evaluation of your symptoms but may need to refer you to a specialist or for in-person treatment. If you are experiencing life-threatening symptoms, seek emergency medical attention immediately.

Learn about gout
Gout is a common and complex form of arthritis. When your body has high levels of uric acid, uric crystals can form in your joints, causing swelling, redness, and severe joint pain.
Gout symptoms can come and go, and ongoing pain can take a toll on your quality of life. Fortunately, treatment options can help you manage symptoms and prevent gout attacks.
Gout causes
Gout, the most common type of inflammatory arthritis, happens when people have high levels of uric acid. The human body naturally produces uric acid during the breakdown called purines. Uric acid flows through the kidneys and exits the body through urination.
When you have too much uric acid, either naturally or from a high-purine diet, it can form urate crystals that lodge in the joints, leading you to develop gout. Some risk factors that can increase your uric acid levels include:Eating a diet rich in red meat, selfish, fruit juice, and alcoholic beverages
Certain medical conditions, such as high blood pressure and kidney disease
Low-dose aspirin and high blood pressure medications
A family history of gout
Older age
Recent surgery or trauma
Gout symptoms
With acute gout, symptoms tend to come on quickly from the buildup of uric acid crystals. Gout attacks can be extremely painful and may happen overnight. During a gout attack, patients typically experience:
Severe pain
Redness
Swelling
Stiffness
Tenderness, even to gentle touch
Warmth, or the feeling that the affected joint is "on fire"
In some cases, people have high uric acid levels in their blood but don't experience any symptoms. This is called asymptomatic hyperuricemia.

How to treat gout
Gout treatment will depend on the stage and severity of your condition. Your treatment plan may include:
Lifestyle changes: For many people, losing weight and eating a balanced diet can help prevent gout flare-ups. Eating a low-sodium Mediterranean or DASH diet, with an emphasis on fruits, vegetables, nuts, and other unprocessed foods, can significantly reduce gout flare-ups.
Prescription medications: If you experience frequent attacks, your doctor may prescribe anti-inflammatory medication or uric acid-lowering drugs to help you manage symptoms.
Gout surgery: In most cases, gout can be treated effectively without surgery. But after many years, hard deposits can build up on your joints, causing permanent damage. Gout surgery removes these deposits to reduce pain.
Gout medications
Depending on your medical history, symptoms, and frequency of gout attacks, your doctor may prescribe medication to treat gout. Some drugs to help control symptoms include:
Nonsteroidal anti-inflammatory drugs (NSAIDs)
Such as ibuprofen (Motrin, Advil), naproxen (Aleve), and indomethacin (Indocin, Tivorbex)
Colchicine (Colcrys, Mitigare)
A prescription anti-inflammatory drug that can help relieve gout pain
Corticosteroids
Which can help reduce inflammation and relieve swelling in the inflamed joint
Uric acid-lowering drugs
Such as febuxostat (Uloric) and allopurinol (Aloprim, Zyloprim), which help lower uric acid levels in the blood

How to prevent gout
Healthy lifestyle choices can help lower your risk factors for gout. These choices include:
Drink plenty of water to avoid dehydration and boost kidney function.
Stay active to maintain a healthy weight. Being overweight or obese increases uric acid levels in your body and creates added stress on your joints.
Limit how much alcohol and sweetened beverages (i.e., fruit juice) you drink.
Only eat purine-rich food, such as shellfish, beef, pork, and organ meat, in moderation.
Limit your purine intake by eating a low-fat, non-dairy diet rich in whole foods.

When to see a doctor for gout
If you experience sudden, severe pain in a joint, talk to your doctor. Without appropriate treatment, gout can lead to gouty arthritis (chronic gout), a more severe form of arthritis. This condition can leave affected joints permanently damaged and swollen.
Seek immediate medical attention if you have a fever and an inflamed joint. These may be signs of a serious infection.
Gout treatment FAQs
What are the symptoms of gout?
The most common symptom of gout is the sudden onset of intense pain in a single joint, usually in the big toe. During a gout attack, you may also experience:
Swelling, redness, and inflammation
Stiffness in the affected joint
Warmth, or feeling like your joint is "on fire"
How do you treat gout?
Treatment options for grout vary depending on the stage and severity of the condition. Many people can effectively manage symptoms with a combination of medication and lifestyle changes.
If you're experiencing intense pain, redness, or inflammation in your joints, book an appointment with one of our board-certified doctors to get gout treatment online. Our board-certified doctors can prescribe prescription NSAIDs (e.g., celecoxib and meloxicam) to reduce inflammation and treat gout. Other prescriptions, including allopurinol, colchicine, and febuxostat, are also available to help lower the levels of uric acid in the blood.What foods I should avoid for gout?
If you have gout, avoiding high-purine foods can help reduce the frequency of gout attacks and lower the uric acid level in your blood. Some foods to avoid include:
Alcohol, especially beer
High fructose corn syrup
Red meat, including pork, lamb, and beef
Oily fish, mussels, and scallops
Where can I get meloxicam for gout?
You can get meloxicam, a prescription-strength NSAID, by booking an appointment with an online doctor. At PlushCare, a board-certified medical specialist can prescribe meloxicam for gout after a video consultation.
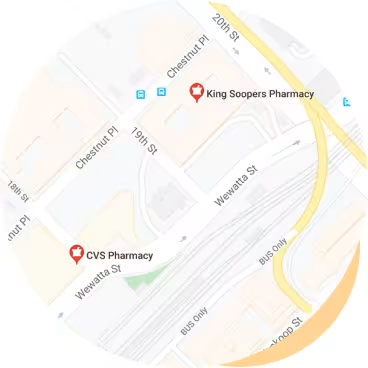
After a quick video consult with an online doctor to diagnose gout, your doctor will review your medical history and symptoms to create a personalized treatment plan. If needed, your doctor can also write a prescription for meloxicam and send it to your local pharmacy.What are the top prescription medications for gout?
The top prescription medications for gout include anti-inflammatory medications and uric acid-lowering drugs, which help manage symptoms and lower the frequency of attacks.
To get online gout treatment, book an appointment with one of our board-certified PlushCare doctors. Once your online doctor diagnoses your gout, they can prescribe medications to treat your symptoms, such as:Allopurinol (Aloprim, Zyloprim)
Colchicine (Colcrys, Mitigare)
Febuxostat (Uloric)
Indomethacin (Indocin, Tivorbex)
Related conditions to gout
Diabetes
Gouty arthritis (chronic gout)
Heart disease
High blood pressure (hypertension)
Kidney disease
3 simple steps to get treated for gout today

Step 1
Book a gout treatment appointment.
Book a same day appointment from anywhere.

Step 2
Talk to your medical provider regarding your gout symptoms.
Visit with a doctor on your smartphone or computer.
Step 3
Pick up a prescription for gout.
We can send prescriptions to any local pharmacy.
Gout treatment pricing details
How pricing works
To request gout treatment and get a new prescription or refill on your prescription, join our monthly membership and get discounted visits.
Paying with insurance
Membership
$16.99/month
First month free
Visits
Copay
30 days of free membership
Same-day appointments 7 days a week
Unlimited messages with your Care Team
Prescription discount card to save up to 80%
Exclusive discounts on lab tests
Free memberships for your family
Cancel anytime
Visit price with insurance
Often the same as an office visit. Most patients with in-network insurance pay $30 or less!
We accept these insurance plans and many more:
Paying without insurance
Membership
$16.99/month
First month free
Visits
$129
30 days of free membership
Same-day appointments 7 days a week
Unlimited messages with your Care Team
Prescription discount card to save up to 80%
Exclusive discounts on lab tests
Free memberships for your family
Cancel anytime
Visit price without insurance
Initial visits are $129.
If we're unable to treat you, we'll provide a full refund.
Gout Resources
Sources:
PlushCare is dedicated to providing you with accurate and trustworthy health information
Arthritis Foundation. Gout. Accessed on July 25, 2022. https://www.arthritis.org/diseases/gout
Centers for Disease Control and Prevention. Gout. Accessed on July 25, 2022. https://www.cdc.gov/arthritis/basics/gout.html#:~:text=Gout%20is%20a%20common%20form,no%20symptoms%2C%20known%20as%20remission.
Cleveland Clinic. Gout. Accessed on July 25, 2022. https://my.clevelandclinic.org/health/diseases/4755-gout
Mayo Clinic. Gout. Accessed on July 25, 2022. https://www.mayoclinic.org/diseases-conditions/gout/diagnosis-treatment/drc-20372903
PlushCare content is reviewed by MDs, PhDs, NPs, nutritionists, and other healthcare professionals. Learn more about our editorial standards and meet the medical team. The PlushCare site or any linked materials are not intended and should not be construed as medical advice, nor is the information a substitute for professional medical expertise or treatment.